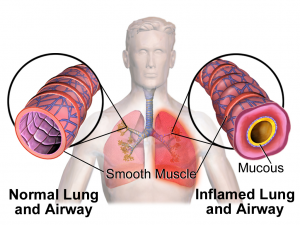
Asthma is a chronic condition characterized by variable airflow obstruction, airway inflammation, and hyper-responsiveness to stimuli. When triggered, the airways become swollen, and the surrounding muscles tighten, making it difficult for air to move in and out of the lungs. Over time, persistent inflammation and injury to the airway linings cause structural changes, leading to worsening symptoms and a decline in lung function.
Asthma, like many other allergic diseases, often runs in families. While many cases are triggered by allergies, asthma can also occur in people without allergies. Common triggers include exercise, viral infections, smoke, temperature and humidity changes, air pollution, strong odors, emotional stress, and occupational exposures.
Symptoms
The most common symptom of asthma is wheezing. However, it can also present with:
- Shortness of breath
- Chest tightness
- Chronic cough
- Nighttime awakenings due to coughing or wheezing
- Easy fatigue or cough with exercise
Diagnosis
After reviewing a patient’s medical history, doctors may order lung function tests to assess breathing. The most common test is spirometry, usually performed in a doctor’s office, to monitor asthma severity and response to treatment. In some cases, additional tests may be needed to measure lung function and airway responsiveness.
Management
Although there is no cure for asthma, symptoms can be effectively managed by avoiding triggers and following prescribed treatments.
Doctors assess asthma severity based on symptom frequency, lung function, and exacerbation history to determine the appropriate medications. Regular follow-ups help adjust treatment to maintain symptom control while minimizing side effects—a strategy known as the step-up/step-down approach.
Medications for Asthma
There are two main types of asthma medications:
- Rescue Medications (Quick-relief)
- Fast-acting bronchodilators (Short-Acting Beta-Agonists or SABAs) provide immediate relief during asthma attacks.
- If rescue medication is needed more than twice a week, a doctor should be consulted.
- Controller Medications (Daily maintenance therapy)
- Inhaled corticosteroids (ICS) – Reduce airway inflammation.
- Combination inhalers (ICS + Long-Acting Beta-Agonist or LABA, and sometimes a Long-Acting Muscarinic Antagonist or LAMA) – Provide both anti-inflammatory and long-term bronchodilation benefits.
- Oral medications (e.g., Montelukast, Theophylline, Cromolyn) – Additional options for asthma management.
- Oral steroids – Used for acute asthma flares but not for long-term use due to side effects.
- Biologic therapies – For moderate to severe persistent asthma that is not controlled with inhaled corticosteroids and bronchodilators. Such biologicals include Omalizumab (Xolair), Mepolizumab (Nucala), Benralizumab (Fasenra), Dupilumab (Dupixent), and Tezepelumab (Tezspire).
Self-Care & Monitoring
Avoid known triggers to reduce the risk of asthma attacks.
Monitor breathing at home using a peak flow meter; a drop of 20% or more from your personal best may indicate worsening asthma.
Use the Asthma Control Test (ACT) for self-assessment. Separate Asthma Control Test versions are available for ages 4-11 and 12 and above.
A score below 19 suggests poor control, and you should notify your doctor.
Useful linkes:
http://www.aaaai.org/conditions-and-treatments/asthma.aspx